NEWS ARTICLE
Immunisation in pregnancy ‘safe’, but uptake still low
Research by a Charles Darwin University PhD graduate shows influenza and pertussis (whooping cough) vaccines in pregnancy are safe for mums and bubs, but uptake remains low.
The research through the Menzies School of Health Research by Dr Lisa McHugh investigated the safety of vaccination in pregnancy, including one study of more than 9000 mothers and infants.
She said that despite nationally recommended flu and whooping cough vaccination in pregnancy programs, uptake has remained sub-optimal across Australia.
“Influenza and pertussis vaccinations are recommended in pregnancy to protect both mother and baby,” Dr McHugh said.
“Pregnant women are more than twice as likely to be admitted to hospital as other people with influenza, while evidence shows pertussis vaccination during pregnancy reduces deadly whooping cough disease in babies who are less than three months by more than 90%.”
Part of the research examined the baseline rates of adverse birth outcomes together with influenza and pertussis infections for the whole of Northern Territory and Queensland population to calculate the burden of disease before the introduction of influenza and pertussis vaccinations in pregnancy.
Dr McHugh said the study included a significant proportion of Aboriginal mothers and babies from the NT and found the disease burden from influenza and whooping cough, and adverse birth outcomes, was much higher in this group.
“We then looked at the rates of adverse birth outcomes in mothers who were vaccinated during pregnancy compared to those who were not,” she said.
“We found no evidence that there was any increase in risk of an adverse birth outcome for infants whose mothers were vaccinated during pregnancy.”
Dr McHugh said one of the most surprising findings centered around the uptake of the influenza vaccine by pregnant Aboriginal women living remotely.
“We had expected the uptake of influenza vaccine would be fairly high but what we actually found was an uptake of under 5%,” she said. “Reasons for this are likely multifaceted but may relate to a lack of evidence of their safety, a lack of cultural appropriation and limited access.”
Dr McHugh said the need to include and collaborate with First Nations people when researching their health barriers and outcomes was vital.
“The research had a significant focus on Aboriginal mothers and babies, with few whole-of-population and policy-relevant immunisation studies having such comparable long-term data,” she said.
“The evidence gained in this study – that immunisation is in fact safe – will, hopefully, contribute to a greater willingness of health care workers and pregnant women to embrace this program, particularly if Aboriginal people are included in decision-making processes at every opportunity.”
Dr McHugh has trained and worked as midwife in Sydney, Queensland and the Northern Territory.
Related Articles

Rooting out plant diseases: Are computers ready to run our farms?
Nature is still too complex for artificial intelligence (AI) modelling to be effective, but the tipping point is close, according to a new study that found the technology may still trip at the last real-world hurdle.
Read more about Rooting out plant diseases: Are computers ready to run our farms?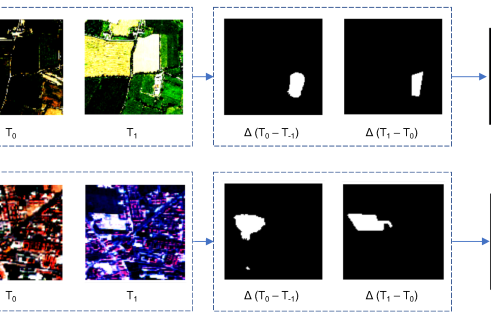
Tech on the treetops: How AI can protect forests
The Artificial Intelligence model was developed to detect changes in forest cover.
Read more about Tech on the treetops: How AI can protect forests
Volunteers protected Darwin wildlife for 50+ years, but new research suggests it’s time to stop winging conservation efforts
Volunteers have shouldered the burden of shorebird conservation in the Top End for more than half a century, but new research from Charles Darwin University (CDU) suggests it’s time for the government to take responsibility for all of the Northern Territory’s residents – including those with wings.
Read more about Volunteers protected Darwin wildlife for 50+ years, but new research suggests it’s time to stop winging conservation efforts
